Knee Pain
Knee pain is a common complaint that affects people of all ages. Knee pain may be the result of an injury, a mechanical issue, or from medical conditions such as arthritis.
Common Knee Injuries and Conditions
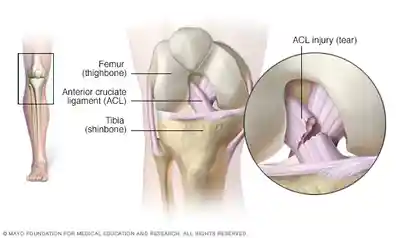
ACL Injury
An ACL injury is a tear or stretch of the anterior cruciate ligament (ACL) — one of four ligaments that help stabilize the knee. It’s main function is to decelerate and stop forward motion and rotation of the shin bone on the thigh bone. Noted to be a very common injury, there are typically between 100,000-200,000 incidents per year in the United States.
An ACL injury is particularly common in people who play basketball, soccer or other sports that require sudden changes in direction. Eccentric quadriceps weakness related to a lesser lower extremity injury, if not properly rehabbed, can lead to an ACL tear. Associated with ACL tears is the less common “Unhappy Triad”, in which one tears the ACL, MCL, and Medial Meniscus.
Symptoms
Pain, swelling, and instability are the most common symptoms with an ACL tear. Upon immediate evaluation, those trained may be able to diagnosed the tear through special tests but typically after several hours due to swelling and guarding it is more difficult to assess and a MRI is usually ordered to diagnose the tear and severity.
When to See a Doctor or Physical Therapist
Depending on the severity of the ACL tear, one may feel or hear a pop, experience immediate swelling and the knee giving out. If you have experienced this, it would be recommended you see your doctor and likely undergo a MRI to confirm the tear and any other associated injuries. ACL tears can be graded I-III, with III being the most severe.
Grade I – the ligament has been stretched but it still does a good job of stabilizing the knee joint and surgery is less likely to be recommended.
Grade II – more rare as the ligament is partially torn and stretched and loosened.
Grade III – very serious as the ligament is torn and most often requires surgery.
If your child or adolescent tears an ACL, surgery is less likely to be recommended since they are still growing and performing the surgery risks growth plate injury, potentially leading to bone growth problems.
Elite Physical Therapy & Sports Medicine’s Treatment for ACL Surgery
Expect to begin therapy 2 days following your ACL surgery. Depending on your surgeon, you may need crutches or a knee brace. Restoring normal knee range of motion, patellofemoral mechanics, strength and function are the focus for this type of injury.
Blood flow restriction can be helpful for those having trouble regaining strength. Dry Needling and Kinesio Tape can be helpful limiting patellofemoral pain. Our Anti-gravity Treadmill (AlterG) is an excellent device to restore normal gait at a much quicker rate than other clinics in this area.
Meniscus Injury
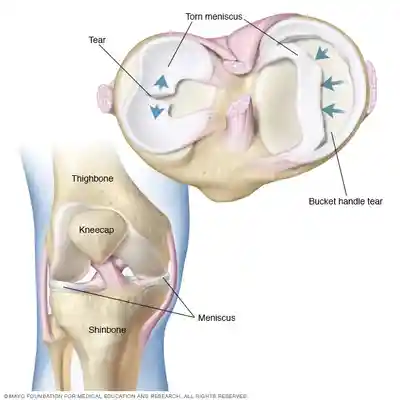
The meniscus a tough, rubbery cartilage that acts as a shock absorber between the upper leg bone (femur) and lower leg bone (tibia). It can be torn if you suddenly twist your knee while bearing weight on it, especially if in a squatted position. The meniscus can also become degenerative over time and tear with no mechanism of injury.
Due to the lack of blood supply to this area, surgery is commonly performed as it will not heal on its own. Sometimes, one may irritate or aggravate the meniscal-capsular junction and feel similar symptoms to a meniscus tear but will heal in time with no surgery required.
Symptoms
One may experience several or none of the following symptoms: A popping sensation, swelling or stiffness, pain (especially when twisting or rotating your knee), difficulty straightening your knee fully, feeling as though your knee is locked in place when you try to move it, and feeling of your knee giving way.
Surgery and Rehabilitation for a Meniscus Tear
Two surgeries that are performed when a meniscus tear is present are meniscectomy and meniscus repair. A partial meniscectomy is most commonly performed on non-athletes and those typically in their mid 20’s and older and involves removing the involved piece of meniscus.
A meniscus repair is typically performed on those younger than 25 and those whom are high level athletes. This method involves sowing/suturing the torn meniscus back to its original position and involves a more lengthy and involved rehabilitation than a meniscectomy.
Regaining normal range of motion, strength, and function are once again the focus of rehabilitation and each rehab program is developed for each individual person.
Patellar Tendonitis
Patellar Tendonitis (also known as jumper’s knee) causes irritation and inflammation to the patellar tendon — the thick, fibrous band of tissue that attaches the quadricep tendon to the tibia. This inflammation can happen when there’s an injury to the patellar tendon, which allows you to kick, run and jump. Runners, skiers, cyclists, and those involved in jumping sports and activities may develop patellar tendonitis. One may also develop the tendonitis after ACL surgery when the patellar tendon is used as the ACL.
Symptoms
Pain along with a dull ache and tenderness around your patellar tendon, swelling, pain with jumping, running, or walking. Pain and stiffness when bending or straightening your leg, and tenderness behind the lower part of your kneecap. Kneeling can also be painful in addition to squatting or descending stairs.
When to see a Doctor or Physical Therapist
Left untreated, the pain and soreness can become debilitating and may lead to a patellar tendon rupture. It has been shown in some cases, repeated overuse over a prolonged period of time can cause the patellar tendon to abruptly tear. You should see your doctor or therapist when the dull ache around the knee lasts long after you stop activity, when you experience sharp, severe pain after sudden movement, and when your pain worsens during activity.
Elite Physical Therapy & Sports Medicine’s Treatment for Patellar Tendonitis
Increasing the blood supply to the affected area is vital for this condition. We have several methods to help provide the necessary blood supply including Graston and Dry Needling among other methods. Kinesio Taping can also be helpful in reducing pain and improving blood flow to the tendon. Applied functional science can also be applied to find the source of why the tendon is becoming inflamed and irritated vs simply treating the symptoms only.

Fractures
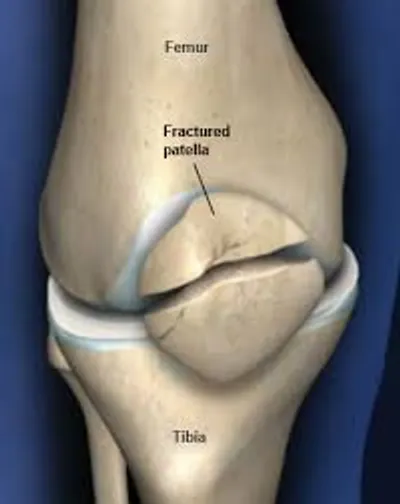
The bones of the knee, including the kneecap (patella), can be broken during falls or auto accidents. Also, people whose bones have been weakened by osteoporosis can sometimes sustain a knee fracture simply by stepping wrong. One would seek medical treatment immediately if a known fracture or severe pain is present.
Symptoms
Pain around the kneecap or in the knee, bruising, swelling (which can be severe, even with relatively minor kneecap fractures), inability to bend or straighten the knee or to hold the leg out straight, inability to bear weight, stand or walk, deformed appearance of the knee (especially with severe fractures), and bone protruding from the skin of the knee in the case of an open patellar fracture.
Elite Physical Therapy & Sports Medicine’s Treatment for Knee Fractures
Depending on the type of fracture, if surgery is required, and what type of surgery is performed, this type of injury is typically treated conservatively in regards to regaining range of motion and WB/ambulation status. Ultimately, full range of motion is typically expected and full recovery although therapy can be several months.
Our Anti-gravity Treadmill (AlterG) can be especially important with this injury as we can get you walking with your weight-bearing restrictions and restoring your normal gait sooner than other clinics in the Greater Lafayette area.
Patellofemoral Pain Syndrome (PFPS)
Patellofemoral pain syndrome (also known as runner’s knee) is a general term that refers to pain arising between the kneecap and the underlying femur bone. It’s one of the most common causes of knee pain as it can occur in athletes; in young adults (especially those whose kneecap doesn’t track properly in its groove); and in older adults (who usually develop the condition as a result of arthritis of the kneecap).
It can also occur indirectly from other knee, hip, and lower extremity injuries that effect quadriceps strength. As the quadriceps looses strength or the timing of the four muscles do not contract equally and at the same time, patellofemoral pain can occur. Muscular imbalances between the quadriceps and hamstrings along with tightness in the hamstrings, Iliotibial Band and calf muscles contribute to more kneecap pain and discomfort.
Problems with patellar alignment, overpronation, changes in footwear, and overuse can also contribute to PFPS.
Symptoms
Pain in and around the kneecap that happens when you are active. Or pain after sitting for a long time with the knees bent. This sometimes causes weakness or feelings of instability. Rubbing, grinding, or clicking sound of the kneecap that you hear when you bend and straighten your knee. Pain with stairs, squatting and kneeling. A kneecap that is tender to the touch.
When to see a Doctor or Physical Therapist
You may want to follow up with a Doctor or Physical Therapist if your knee pain persists after activity or exercise, with stairs, or when sitting for prolonged periods of time.
Elite Physical Therapy & Sports Medicine’s Treatment for PFPS
Reducing the tight extensor musculature, improving patella mobility, and increasing quadricep strength and timing are the focus with this condition. Kinesio Taping is beneficial in controlling the patella and maintaining its proper position while reducing pain, allowing you to perform daily activity with less pain and popping.
Neuromuscular re-education (NMES) is helpful in regaining the proper timing/firing of the four quadriceps muscles. NMES applied with Blood Flow Restriction can be very powerful in regaining the strength early after injury. Applied functional science can be applied to help find the source of why the symptoms are occurring and improving global mobility and stability.

Iliotibial Band Syndrome (ITBS)

This syndrome occurs when the wide, tough band of tissue that extends from the outside of your hip to the outside of your knee (iliotibial band) becomes so tight that it rubs against the outer portion of your thighbone as well as the insertion point on the lateral knee. Marines in training (20%), distance runners (12%), and cyclists are especially susceptible to iliotibial band syndrome.
Symptoms can be in the lateral thigh, lateral knee, or both. A snapping sensation may also be felt. Many people confuse this lateral pain with hip arthritis or hip joint pain, which causes pain to the inside of your hip or groin. If the pain persists and doesn’t improve in a few weeks or worsens, you should seek medical advice.
Symptoms
Hip pain: Your iliotibial band repeatedly rubs against your greater trochanteric in your hip. Your greater trochanteric is where the bone widens near the top of your femur. The friction causes inflammation in your tendon and pain in your hip. You might hear a snapping sound over the greater trochanter.
Knee pain: Occurs in 25% of adults. Your lateral epicondyle is on the outside of your knee near the bottom of your femur, where the bone widens. Your tense iliotibial band repeatedly rubs against your lateral epicondyle of the knee when you flex and extend your knee. The friction causes inflammation in your tendon and pain in your knee. The outside of your knee might look discolored and feel warm to the touch. You might feel a snap, pop or click on the outside of your knee.
At first, the pain will start after you exercise. As the syndrome worsens, you’ll feel it before and after you exercise, and ultimately the entire time you exercise and, eventually, also when you’re resting.
Elite Physical Therapy & Sports Medicine’s Treatment for ITBS
Restoring normal tissue extensibility and mobility of the Iliotibial band are key as well as improving stability of the hip. Identifying the source of tightness thru Applied functional science (which can be on the other side of the body) is also considered. Excessive foot pronation and hip abductor weakness can be contributing factors for ITBS that can be evaluated.
Graston, Dry Needling, Kinseio Taping, and manual therapy are all helpful with this condition. We also offer lower extremity compression therapy that is beneficial in improving blood flow and returning the muscle to its normal tissue extensibility.
For runners who need to continue to train for their upcoming race and can’t afford to stop training, our Anti-gravity Treadmill (AlterG) is perfect for unloading stress to the iliotibial band and avoiding further injury.
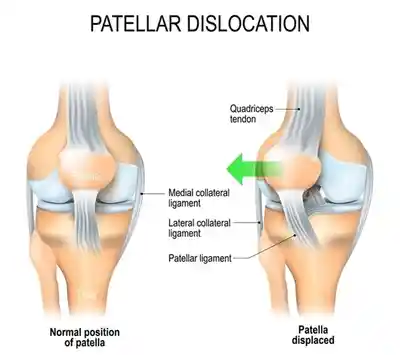
Patellar Dislocation (Dislocated Kneecap)
This occurs when the triangular bone that covers the front of your knee (patella) slips out of place, usually to the outside of your knee (93% of the time). In some cases, the kneecap may stay displaced and you’ll be able to see the dislocation. It usually occurs by force, from a collision, or from a fall. Most often, you will not be able to walk unless the patella pops back into place.
Symptoms
- Audible pop, locking of the knee, kneecap visually out of place
- Intense pain, buckling of the knee, sudden swelling, inability to walk
When to see a Doctor or Physical Therapist
Although not life threatening, you should seek immediate medical attention if you have dislocated your patella and it remains dislocated. Once reduced or relocated, your physician should refer you to physical therapy to begin restoring your range of motion and strength while protecting your patella.
Elite Physical Therapy & Sports Medicine’s Treatment for Patellar Dislocation
Restoring your range of motion, gait, and strength while protecting the patella is the main focus with this type of injury.
Neuromuscular electrical stimulation (NMES) along with Blood Flow Restriction (BFR) can be extremely effective in restoring strength and proper timing to the quad muscles, particularly the VMO which is helpful in limiting the patella moving or shifting lateral. Kinesio Taping can be utilized as you progress and begin more weight-bearing and normal activities of daily living (ADL’s).
If your pain persists and you need to get back to running or jogging, our anti-gravity treadmill (AlterG) is extremely successful in restoring normal stride and speed without the pain and at a much faster rate of return than a normal treadmill.
Osteoarthritis and Total Knee Replacement
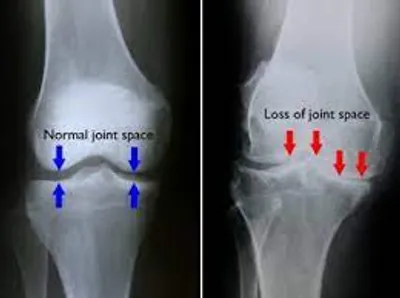
Sometimes called degenerative arthritis, osteoarthritis (OA) is the most common type of arthritis. It’s a wear-and-tear condition that occurs when the cartilage in your knee deteriorates with use and age. Your medical provider can determine the level of severity through x-rays and your pain level with normal activities of daily living (ADLs). If severe and bone on bone is noted on the x-rays, a total knee replacement (TKR) may be recommended if you are also experiencing moderate-severe pain with ADLs.
Symptoms
Unlike other forms of arthritis, OA usually develops gradually over many months and years. Pain and joint swelling typically increase over time as well. Pain typically is experienced with getting out of a seated position, stairs, squatting, and other weight-bearing activities.
When to see a Doctor or Physical Therapist
It is best to see a physical therapist when you first start to experience any knee pain in hopes to decrease pain and prolong life of the knee joint. If the pain becomes more severe and interferes with normal life, you should see your physician and get x-rays. If severe enough, a total knee replacement will likely be recommended.
Elite Physical Therapy & Sports Medicine’s Treatment for Total Knee Replacement
Depending on the doctor, we may see you for a one-time pre-operative visit to discuss what to expect regarding the surgery, incision, bathing, pre and post-operative instructions and exercises along with what to focus on immediately after surgery.
Post-operatively, we will typically see you 2-3 days after surgery and begin restoring your range of motion (ROM). Early on, it is critical to regain your ROM, particularly knee extension. Blood Flow Restriction (BFR) and neuromuscular stimulation (NMES) is often used early on as well to improve your strength significantly quicker than without.
As your motion and gait improves, focus will shift to improving function and ADLs with strengthening and balance activities. Our anti-gravity treadmill can be useful with those struggling to return to pain-free normal gait.
Less Common Knee Conditions
Loose Body
Sometimes injury or degeneration of bone or cartilage can cause a piece of bone or cartilage to break off and float in the joint space. This may not create any problems unless the loose body interferes with knee joint movement, in which case the effect is something like a pencil caught in a door hinge.
Symptoms
Inability to fully bend or straighten the knee is common. Persistent pain inside the joint may also be present.
When to see a Doctor
You should follow up with your doctor if you experience these type symptoms and your surgeon will likely proceed with an arthroscopy to remove the loose body and referred to physical therapy.
Elite Physical Therapy & Sports Medicine’s Treatment for Loose Body Removal
Physical Therapy is not always recommended or needed with this type of surgery, but anytime you have a surgery, it would be beneficial to see a physical therapist to assess your strength, gait, and motion in addition to any substitution patterns you may have developed. If needed, our therapists would develop a treatment plan to address any issues and therapy would likely be minimal compared to other knee surgeries. You should expect to begin therapy 2 days following your surgery.

Rheumatoid Arthritis
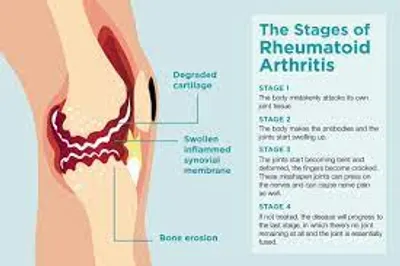
The most debilitating form of arthritis, rheumatoid arthritis is an autoimmune condition that can affect almost any joint in your body, including your knees. Although rheumatoid arthritis is a chronic disease, it tends to vary in severity and may even come and go.
Gout
This type of arthritis occurs when uric acid crystals build up in the joint. While gout most commonly affects the big toe, it can also occur in the knee.
Pseudogout, often mistaken for gout, is caused by calcium-containing crystals that develop in the joint fluid. The knees are the most common joint affected by pseudogout.

Septic Arthritis

Sometimes your knee joint can become infected, leading to swelling, pain and redness. Septic arthritis often occurs with a fever, and there’s usually no trauma before the onset of pain. Septic arthritis can quickly cause extensive damage to the knee cartilage. If you have knee pain with any of the symptoms of septic arthritis, see your doctor right away.
